PAF project
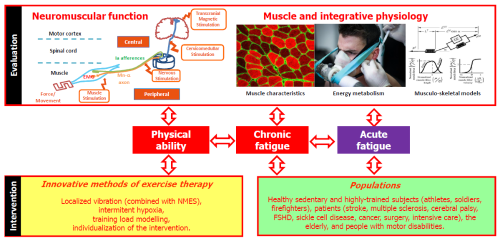
General scientific outline of the PAF team.
While studies on isolated muscle have made it possible to determine the mechanisms and metabolites involved in muscle fatigue, their results are conflicting and their interpretation are still the subject of debate. As a matter of example, we can cite the effects of proton and lactate. These latter have been presented as playing a minor role in fatigue or even a protective role against fatigue, while other studies suggest deleterious effects of these metabolites on muscle function. In humans, fatigue during intense and maximal exercise is often concomitant with acidosis and lactate accumulation. During the next five years, the role of pH and lactate in central and peripheral fatigue will be investigated. Their consequences on neuromuscular function (notably measured in dynamic conditons via force/speed/power/endurance profiles), muscle stiffness and performance will be determined. On the other extremity of the intensity-duration relationship, we will also investigate the environmental (thermal, sleep) and physical constraints for "extreme athletes" (ultra-trailers or soldiers in operation for example) as these parameters induce major physical and cognitive fatigue. One objective will be to identify and understand the perceived, neuromuscular and cognitive fatigue endured by these athletes.
Fatigue is the most commonly reported symptom in many chronic diseases. For example, fatigue affects up to 80% of people with multiple sclerosis, and up to 60% of them consider it as the most disabling symptom. Similarly, 1/3 of cancer patients complain about fatigue months or even years after the end of treatment. In SCD, fatigue is very often described and reported by patients, but still has not received much attention from clinicians. Chronic fatigue is defined as a “subjective lack of physical and/or mental energy, perceived by the individual or the caregiver, which interferes with daily life activity”. It differs from fatigue observed in healthy people by its debilitating nature and by the fact that it is not relieved by rest and sleep.
Neuromuscular fatigue is associated with a decrease of an individual's maximum physical capacity. More precisely, neuromuscular fatigue is defined as a contractile response (force) less than the one expected for a voluntary contraction or a given stimulation. This “inadequate” functional response is due to central (i.e. cortical and/or spinal/motoneuronal) and peripheral (i.e. downstream the neuromuscular junction) processes. Surprisingly, only a few studies have explored the association between neuromuscular fatigue and chronic fatigue. However, less resistance to exercise-induced fatigue can contribute, by repeating daily tasks, to fatigue accumulation and thus to chronic fatigue. Chronic fatigue can also reflect deconditioning (structural and energetic remodeling) or muscle spasticity, or even more general deconditioning such as alteration of the cardiovascular and/or respiratory system, for example. These deconditionings can be either directly (structural muscle remodelling resulting in loss of strength) or indirectly (physical inactivity or pain) linked to the disease, or to age. Therefore, the aim of our research will be to better understand the mechanisms of chronic fatigue, in particular the role of less resistance to neuromuscular fatigue during physical exercise, lower physical ability or muscular remodelling in different pathophysiologies. Seven populations will be particularly studied: elderly, patients with SCD (Messonnier et al. 2019, Ravelojaona et al. 2015), multiple sclerosis (Féasson et al. 2006, Twomey et al. 2017), cancer (Twomey et al. 2018), cerebral palsy (Dohin 2017, Dohin 2019), having stayed in ICU (in collaboration with DeReM-ES team), and after knee surgery (leg ligamento- or arthroplasty). The impact of drug on physical fitness and muscle function, sometimes harmful (as is the case in cancer) and sometimes positive (as is the case with hydroxyurea in SCD), will be investigated. These studies will also be supplemented by investigations on the role of sex (protective effect of a higher residual HbF level in sickle cell patients for example) on chronic fatigue and its causes. A spastic muscle model and evaluation of neurological treatments (neurotomy type) will be developed.
Regular physical activity is a broad spectrum treatment. Indeed, in many chronic diseases, individually calibrated physical activity constitutes a real therapeutic strategy, including in SCD. It has recently been highlighted that an 8-week tailored training program was able to counteract the deleterious effects of the disease on the muscular tissue and to improve the patients’ quality of life (Gellen et al. 2018). In the next five years, the long-term effects will be investigated and one of the objectives pursued will be the establishment of therapeutic recommendations. Better knowledge of mechanisms responsible for muscle weakness and fatigability (see above) will allow us to optimize intervention strategies in rehabilitation/reconditioning or exercise therapy. Among the possible strategies, muscle or tendon localized vibrations have all been shown to be effective in increasing, through neural adaptations, the force production capacities of various muscle groups (for a review, see Souron et al. 2017) including knee extensors (Souron et al. 2018). From now on, the objective will be to offer recommendations for the use of localized vibration in various conditions such as post-operative rehabilitation of the ACL or total knee replacement surgery (collaboration with the SPIP team). The complementarity of vibration with other stimulation modalities such as neuromuscular electrostimulation will also be considered.
Regarding other innovative strategies, recent studies have suggested that exercise in hypoxia could be an effective therapeutic tool for pathological populations. Among various possible strategies, the repetition of sprints in hypoxia is a training method that allows great improvements in resistance to performance degradation during exercise. Currently applied in healthy subjects and high-performance athletes, these training methodologies involving hypoxia could also be used for the rehabilitation of people with loss of autonomy or patients with chronic fatigue. However, before considering such applications, the underlying mechanisms require further investigation (Peyrard et al. 2019). In particular, muscle energy metabolism (measured in NMR), biological (oxidative stress) and vascular markers, muscular perfusion and neuromuscular function will be assessed during different conditioning protocols/training involving hypoxia. To quantify the effects of physical activity, a pharmacodynamic model describing the action of a drug on the body (associating its concentration with a measure of its effectiveness) has been developed. This new approach allows to quantify the dose-effect relationship of physical activity showing an optimal dose beyond which the benefit is reduced because of the induced fatigue (Busso 2017). To show that this type of modelling can be a tool to help the design of an adapted physical activity program, the effects of a brisk walking program for elderly people living in institutions and of a rehabilitation program in coronary patients will be studied (collaboration with EPIS-SNA-laboratory).